Immunotherapy May Offer Ray of Hope for Triple Negative Breast Cancer Patients
- News
- 3.5K
Breast cancer is the most common cancer among women worldwide with over two million new cases diagnosed in 2018. There are different types of breast cancers, mainly classified based on the expression of certain proteins like Estrogen Receptor (ER), Progesterone Receptor (PR) and Her2 (human epidermal growth factor receptor 2).
Drugs have been specifically developed to target these proteins on cancer cells. For example, women with ER-positive breast cancer are treated with a drug called Tamoxifen which blocks the action of ER and has given hope to millions of women. Some breast cancers, however, do not express any of these three proteins (ER, PR or Her2) and are classified as Triple Negative Breast Cancer (TNBC).
TNBC is a notoriously aggressive form of breast cancer and those suffering from it have a slim chance of survival. It is more likely to occur in younger women. This type of breast cancer accounts for approximately 15% of total breast cancer cases. Its incidence in India, however, is higher (27.9%) compared to other regions of the world.
Traditionally, chemotherapy which involves administration of a range of drugs to prevent cancer cells from uncontrolled growth has been the standard of care for TNBC. Despite treatment, TNBC patients show high rates of the reappearance of the disease which unfortunately leads to untimely death. Hence there is an urgent need for better therapies in treating TNBC.
Immunotherapy, which boosts the immune system of the body, has shown a great deal of promise in treating certain cancers and is now being recognized as a potential therapeutic approach in TNBC too. It uses the body’s own molecules or synthetically produced substances that enhance or restore the immune system.
One recently developed type of immunotherapy uses a class of drugs called checkpoint inhibitors, which exploits key surface molecules on T cells, which are a major weapon of the human body’s immune system. James P Allison and Tasuku Honjo were awarded the 2018 Nobel Prize in Physiology or Medicine for their work that led to the discovery of novel molecules which led to the development of immunotherapy.
A new study published recently in New England Journal of Medicine (NEJM) by Dr. Peter Schmid of Barts Cancer Institute, Queen Mary University of London, and his colleagues, has found that combining immunotherapy with chemotherapy could improve the outcome for some advanced triple negative breast cancer patients.
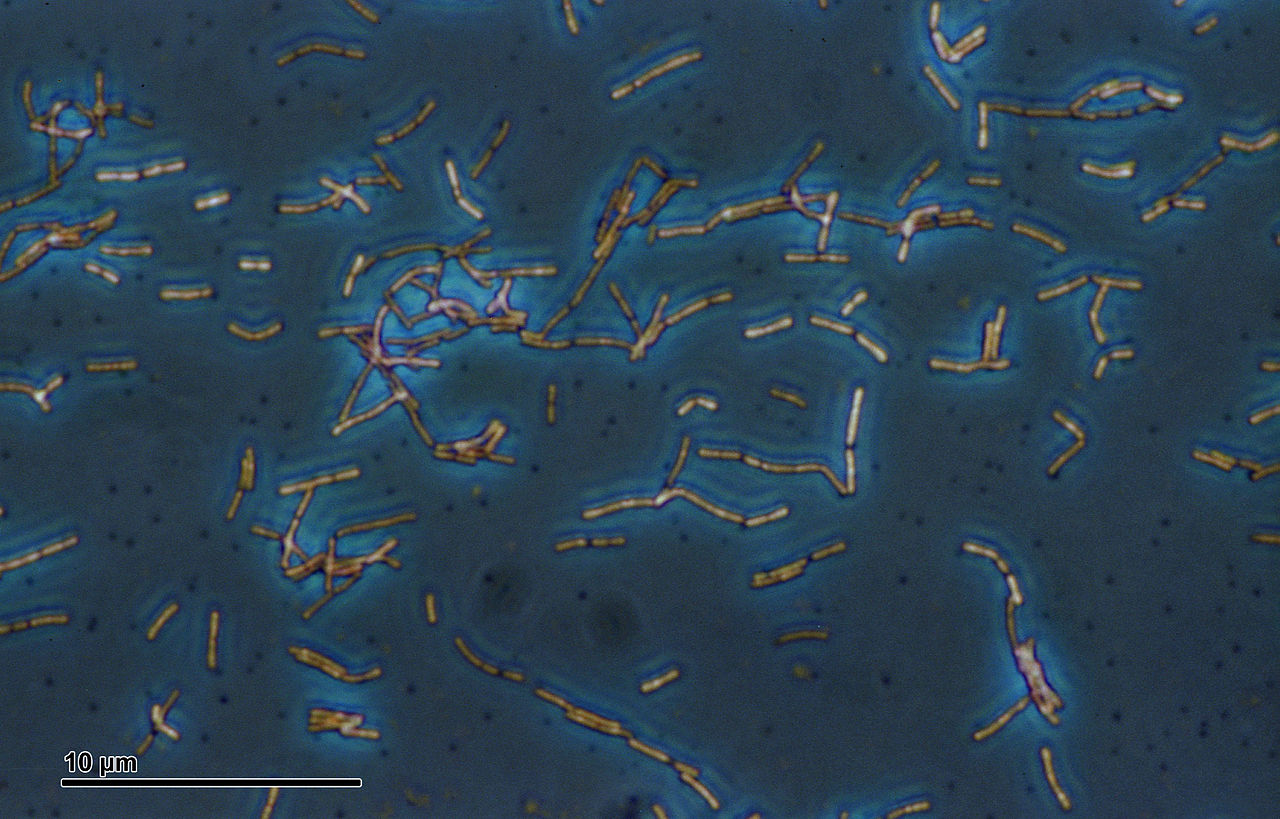
More than 900 patients with untreated metastatic (where cancer has spread to other parts of the body like the lungs) TNBC were enrolled in phase III clinical trial and randomly assigned to receive Nab-Paclitaxel, a chemotherapeutic drug used to treat breast cancer either with a placebo (no immunotherapy drug) or in combination with Atezolizumab, a drug belonging to the checkpoint inhibitor class of immunotherapy drugs.
In the body, immune T cells express a surface molecule called PD-1 which can attach with another molecule called PD-L1 present on other cells. This attachment conveys to T cells that the other cell is not to be destroyed and hence prevents them from being attacked by the immune system. Some cancer cells very cleverly exploit this in a Trojan horse-like manner by having more PD-L1 molecules on their surface and hence escape an immune attack. The immunotherapy drug, Atezolizumab, works by blocking PD-L1 molecules on cancer cells and thus prevents them from conveying wrong signals to immune cells.
However, there are significant drawbacks in this study. The combination therapy was found to increase the average survival to 25 months as against 15.5 months. But cancer cells had to have a high level of PD-L1 molecules on their surface which may not be so in all patients. This means there is a need to check the status of the PD-L1 receptor in patients before commencing the therapy.
In addition, it must be considered that side effects associated with combination therapy are more severe than for single-agent chemotherapy. Also, the cost of such personalized immunotherapy could be extremely high with one round of therapy being Rs. 1 lakh to Rs.13 lakh.
Immunotherapy is still evolving in developing nations like India and is now being offered in just a few treatment centers and that too primarily for solid tumors like prostate, breast, renal, colon, hepatocellular carcinoma, colorectal, oral, lung and ovarian. Although this is only the first large clinical trial involving immunotherapy and more studies are required, the positive findings shine a ray of hope for TNBC patients. (India Science Wire)
(The writer is a Ramanujan Faculty Fellow at the Rajiv Gandhi Centre for Biotechnology, Thiruvananthapuram.)
If you liked this article, then please subscribe to our YouTube Channel for the latest Science & Tech news. You can also find us on Twitter & Facebook.