New Dipstick Urine Test Can Predict Drug Response in Alcoholic Hepatitis
- News
- 1.8K
A group of Indian and French researchers has identified a biomarker in human urine that may help develop a simple test to let clinicians predict response to treatment prior to starting therapy for patients of Severe Alcoholic Hepatitis (SAH). This will help avert risks involved in giving steroid treatment to patients who are not likely to benefit from it.
Prof SK Sarin (R) and Dr. Jaswinder Singh (L)
SAH is caused due to chronic alcohol abuse. It progresses fast and results in death in 60 percent of cases. Unlike Hepatitis B and C which are treatable with drugs, therapeutic options for SAH patients are limited. Corticosteroid therapy is available but not all patients respond to it.
Those who do not respond to steroid therapy have a high risk of infections and may die within three months. That’s why patients need to be classified clinically to predict likely response to steroid treatment.
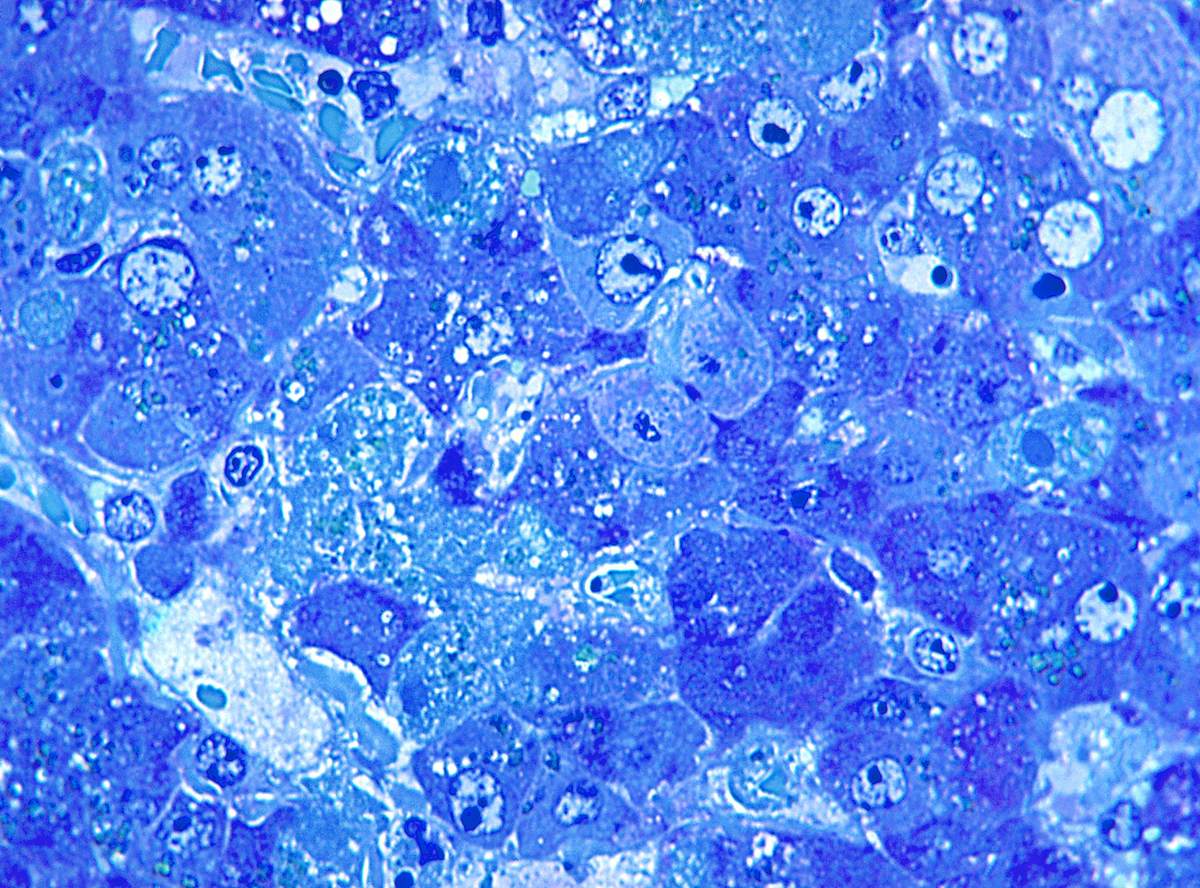
In the new study led by researchers at the New Delhi-based Institute of Liver and Biliary Sciences (ILBS), scientists collected baseline data about urine metabolome in 140 patients of SAH using ultra-high performance liquid chromatography and high-resolution mass spectrometry.
Patients were put on steroid treatment and categorized as responders and non-responders based on a parameter called Lille score after one week of treatment. Further analysis identified certain urine metabolites that were significantly high in non-responders.
A total of 212 features were annotated and identified using various metabolomics and biochemical databases for metabolite identification. The analysis helped zero in nine urinary metabolites prominent in non-responders. These metabolites significantly correlated with severity indices (like MELD or Model of End-stage Liver Diseases) and mortality.
Based on all this data and analysis, researchers have concluded that one particular urinary metabolite – acetyl-L-carnitine – can be used as a biomarker to predict non-response. “Acetyl-L-carnitine at a level of less than 2500 nanogram per milliliter could reliably segregate survivors from non-survivors,” Jaswinder Singh Maras, who conducted the study, told India Science Wire.
“We also assessed if changes in urine metabolome in patients with SAH were linked to alterations in liver gene expression. This highlighted that the change observed in the urine metabolome corresponds to the liver anomaly,” he added.
The results of the study have been published in the journal Hepatology Communications.
“Acetyl-L-carnitine is a noninvasive marker and its quantitation in the urine of SAH patients could help clinicians to categorize at the time of presentation (baseline) patients who have a high predisposition to non-response and non-survival. This could provide a window of opportunity to clinicians to treat these patients differently as compared to those who may respond to treatment,” explained Dr. Shiv Kumar Sarin, director of ILBS.
The scientists at ILBS now plans to customize a dipstick test which will be cost effective for prediction of non-response to corticosteroid therapy and survival chances of patients.
“This study is the first demonstration of the utility of urine to determine treatment responsiveness in SAH. These findings could form the basis for the development of a cost-effective dipstick screening test for restricting steroid use to patients with a good likelihood of responding.
Such a urine test for SAH could provide a practical point of care assessment that may delineate metabolic changes, predict mortality, and potentially personalize treatment strategies,” commented Dr. Shilpa Chokshi (Institute of Hepatology, Foundation for Liver Research, UK) in an editorial comment in the journal. However, she said, the findings need to be confirmed and replicated with patients from different centers worldwide.
In addition to Dr. Sarin and Dr. Maras, the research team included Dr. Sukanta Das, Dr. Shvetank Sharma, Dr. Saggere M. Shasthry (ILBS, New Delhi); Dr.Benoit Colsch, Christophe Junot, (Department of Pharmacology and Immunoanalysis, CEA-Saclay, University of Paris) and Richard Moreau (Center for Research on Inflammation, Paris). (India Science Wire)
By Dinesh C Sharma
If you liked this article, then please subscribe to our YouTube Channel for the latest Science and Tech news. You can also find us on Twitter and Facebook.


